25 June 2024
Making mRNA treatments accessible to low-income countries
Research into mRNA as a therapeutic has shown it to be a highly effective treatment for cancer, respiratory issues, and more, compared to traditional protein-based vaccines. mRNA shows promise as a route to meeting Millenium Development Goals to eradicate problematic, widespread diseases, and hundreds of clinical trials involving mRNA are taking place today with the hope that it will become the standard treatment for a number of diseases and conditions from cancer, to malaria, zika virus, dengue, HIV and many others.
mRNA has already proven to be a rapid and effective treatment in real-world conditions, most notably for COVID-19. As a result, companies are betting on this new technology as the key to solve many untreated conditions
Despite the prolific success of its use across the globe, low-income nations still do not have equitable access to mRNA treatments, primarily due to cost concerns. With a single mRNA vaccine costing dollars compared to cents for traditional vaccines, these nations have been priced out of the market. The impact of this cost barrier could be devastating. Nations can’t provide the healthcare their people need today, and this could result in the spread of deadlier, resistant mutations.
It’s a vicious cycle which can only be staved off by global healthcare equity. In this article, I explore why the cost of mRNA is so high today and what can be done to remove this barrier, and how Cocoon can play a part.
The lessons learned from COVID-19
Traditional vaccinations take between 5 to 10 years to be researched and developed, manufactured and commercially delivered. This is due to several factors, including compliance processes and the complexity introduced by disease mutation.
The COVID-19 pandemic caused organizations to accelerate this process. The speed and global nature of the spread spurred governments, pharmaceuticals, manufacturers and more to collaborate and pour investment into the delivery of an effective vaccination. This included supporting low-income nations that could not offer the same investment.
However, this collaborative spirit was short-lived. Once the dust settled, this collective effort stopped, leaving developing countries without support. The majority of high-income countries are now dispensing the third round of injections and boosters. In contrast, less than 30% of people in low-income countries have received even a single vaccination.
While Covid might not have been as critical in some countries, the fact is that developing nations cannot afford to buy an equitable share of mRNA vaccines, or more specifically, the materials needed to develop them.
Why mRNA is inaccessible to low-income countries
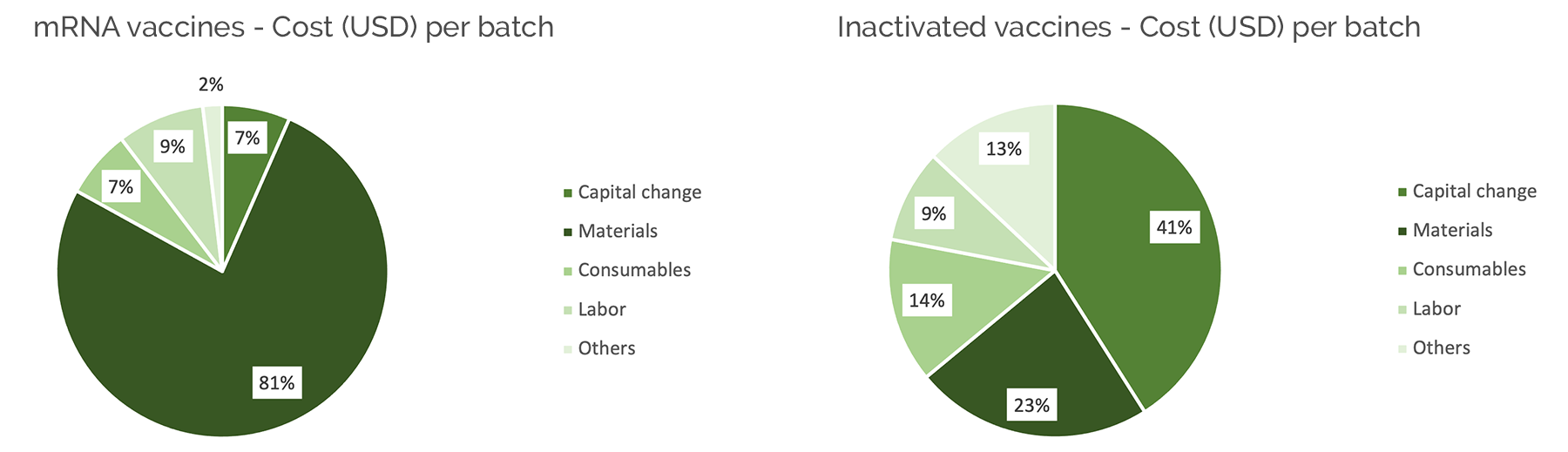
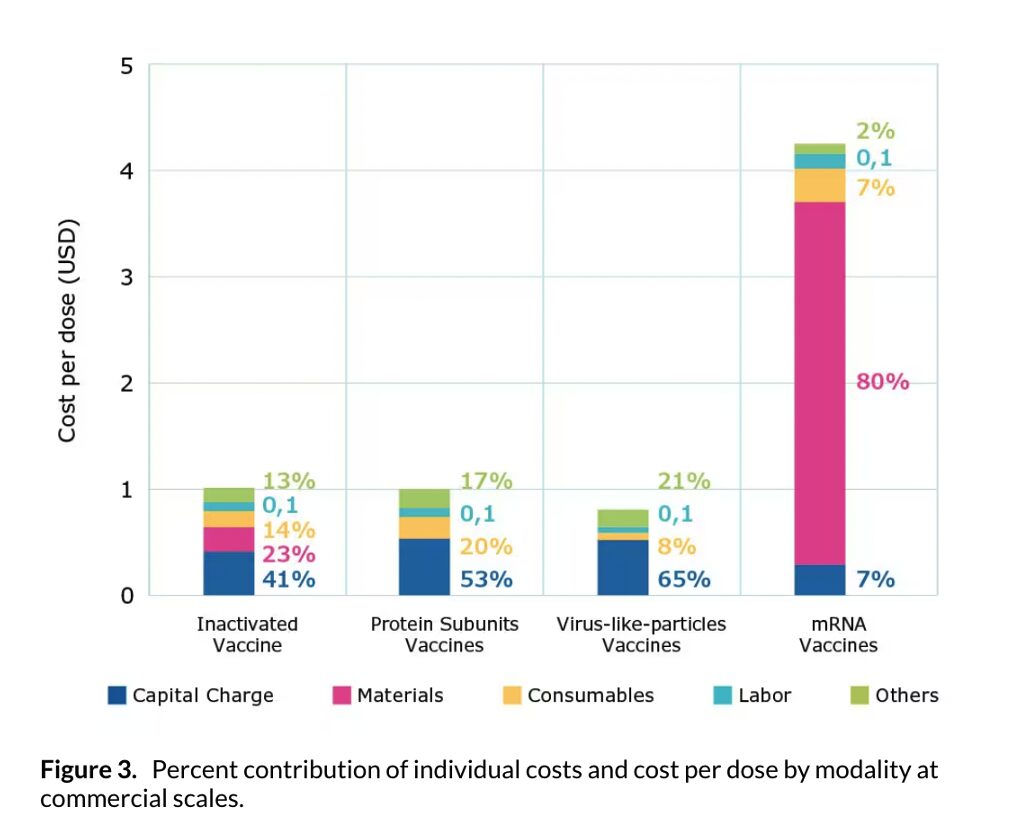
Traditionally, single doses of vaccines cost cents. mRNA doses greatly exceed this. For example, the COVID-19 vaccine costs between 5 to 12 dollars. This is because the cost for materials is so high. Where 80-90% of traditional vaccination costs are spent on manufacturing, maintenance and labor, raw materials make up the same percentage of mRNA vaccine production costs.
| COVID-19. VACCINE 2024 | ||
| Presentation | Supplier | Price |
| Five dose vial, liquid formulation | Janssen | $7,50 |
| Single dose vial, liquid formulation | Pfizer | $12,15 |
| Ten dose vial, paediatric, for dilution | Pfizer | $6,70 |
Source: Unicef
Source: Merck
Low-income countries simply can’t take on these costs at any scale, and especially not for the volume of vaccinations that a pandemic like COVID-19 requires.
1. The cost of enzymes
One of the primary culprits is enzyme costs. Not only are enzymes notoriously expensive to manufacture and purchase, but mRNA vaccinations use significant amounts of enzymes. For example, Moderna’s COVID-19 vaccination uses 341g of Pyrophosphatase per 100 million doses. At $500,000 per 1g, we can see how the costs quickly escalate.
Source: Merck
2. Manufacturing processes aren’t standardized
Complicating this issue is a lack of standardization in enzyme cost and usage. Several of the enzymes used in the process, like pyrophosphatase, cost between $500,000 to $2,000,000 per gram, and other organizations may use fewer or more enzymes in the production of mRNA vaccinations.
Some vaccines will therefore be more expensive to produce, and purchase, than others. This lack of standardization essentially means low-income countries are not protected against higher, exclusionary costs.
3. The manufacturing processes don’t exist
Most major manufacturers for enzymes are located in high-income countries such as the US, Belgium, Germany and UK. Traditionally, low-income countries have relied on compassionate relief to access vaccinations. This means they don’t have the infrastructure to produce the enzymes or vaccinations themselves – and they can’t gain the relief to build it. Although some effort has been made to move production to some African countries, and some companies such as BioNtech are investing in such initiatives, the reality is that developing countries must rely on imported goods.
How can we enable equitable access?
COVID-19 demonstrated the power of collective action.
We need international and cross-industry collaboration, including funders, manufacturers, health organizations, governments, and more, to work together to improve access.
More importantly, we need to support these countries to have financial independence when it comes to healthcare. By reducing the cost of enzymes, nations could afford to import or produce their own vaccines at a cost that is viable at scale.
Cocoon’s new approach to enzyme development meets these needs. Our cost-effective method for producing recombinant proteins for mRNA is >90% more affordable than current market prices. It’s also rapid to develop and manufacture new enzymes while showing high activity. By simplifying the process to achieve easy, linear scalability, we can further contribute to cost reductions and building a more robust supply chain for these critical raw materials.
At these prices, low-income countries could more easily afford equitable and independent mRNA-based treatments, from vaccinations to therapeutics. It would allow nations to treat those in need now and to future-proof themselves against potential threats.
More than this, we want to explore opportunities to collaborate with other organizations and deliver these solutions on a large scale. We are interested in talking to charitable organizations like Path, government initiatives like Gavi, and any other mission-driven alliance to understand how we can contribute to the more affordable production of mRNA treatments for low-income countries.
We believe everyone should have equitable access to innovative and life-saving healthcare – and we are joining the conversation about what can be done.
Learn more about our platform and how it’s reducing costs, here.


